While a herniated disc can be painful and disruptive, many cases resolve without surgery. Knowing the signs, understanding your options, and seeking care early can help you get back to normal activity faster and reduce the chance of recurrence.
Back pain is one of the most common medical complaints in the United States. For many, the culprit is a herniated disc. Whether you’re dealing with sudden discomfort after lifting something heavy or noticing persistent numbness or weakness in your legs, questions about disc injuries come quickly. Can it get better on its own? Will you need surgery? How long will recovery take?
At Georgia Neurosurgical Institute, our team has decades of experience treating patients with spinal disc issues of every kind, from mild disc bulges to complex, multi-level herniations. In this article, we’ve answered some of the most frequently asked questions about herniated discs so you can better understand what’s happening in your body and when to seek expert care.
Can a Herniated Disc Heal on Its Own?
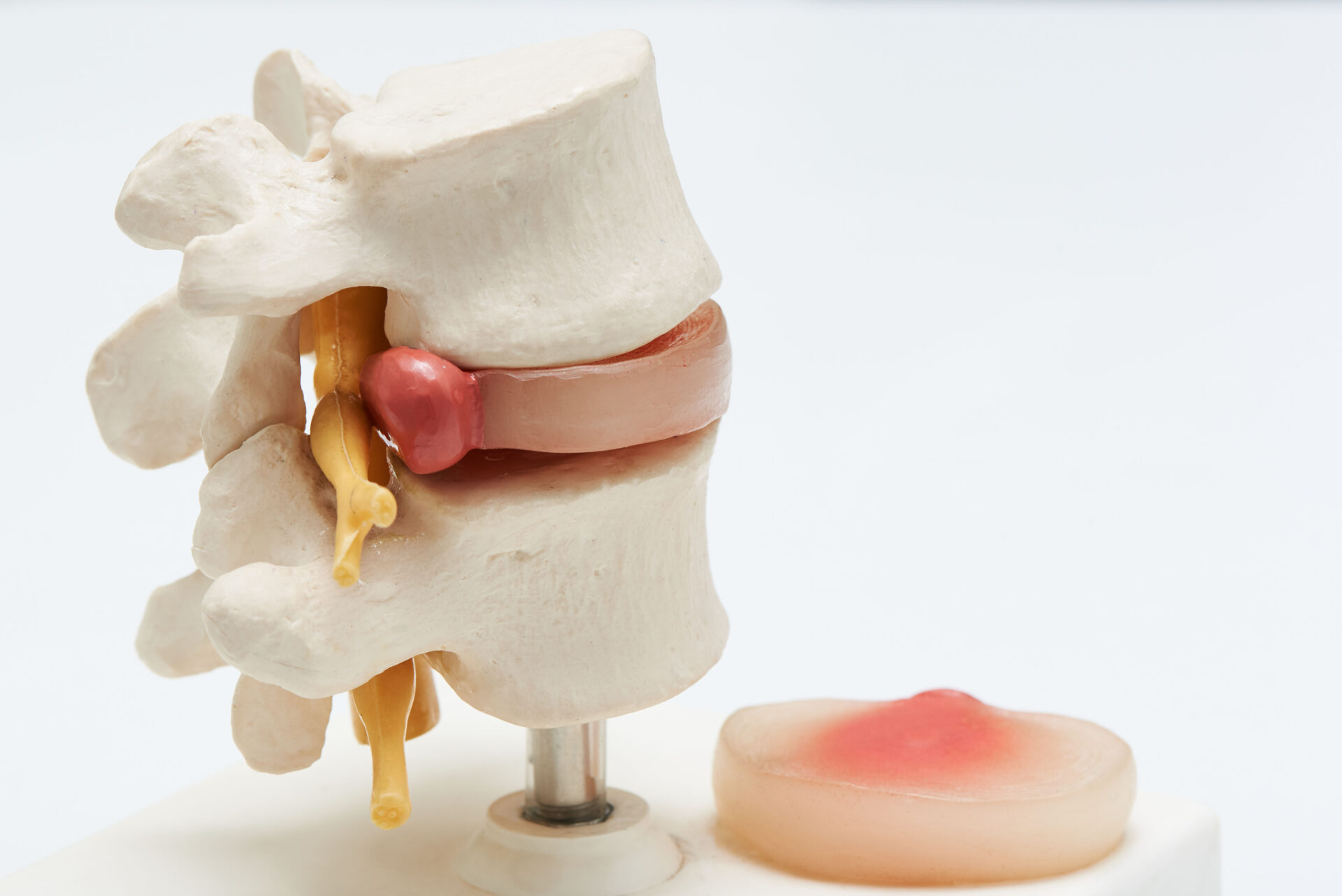
In many cases, yes. A herniated disc can sometimes heal on its own with rest, physical therapy, and non-surgical care. The outer portion of the disc (the annulus) may eventually reabsorb the displaced inner gel (nucleus pulposus), relieving pressure on nearby nerves. This process, called resorption, can take several weeks to several months, depending on the severity of the herniation and the individual’s overall health.
Not all herniated discs follow this path, however. If symptoms persist or worsen, medical intervention may be necessary.
What Are the Most Common Symptoms of a Herniated Disc?
Symptoms vary depending on where in the spine the herniation occurs and whether a nerve is compressed. For example, a herniated disc in the lower back (lumbar spine) may affect the sciatic nerve, while a disc in the neck (cervical spine) could lead to shoulder and arm symptoms.
Typical signs include:
- Pain that radiates to the arms or legs
- Numbness or tingling in extremities
- Muscle weakness
- Pain that worsens with movement or certain positions
- Loss of coordination or balance (in severe cases)
Pain doesn’t always appear at the site of the disc. For example, a herniated lumbar disc may cause pain down one leg, a phenomenon known as sciatica.
What Causes a Herniated Disc?
The most common cause is disc degeneration, or age-related wear and tear on the spine. As discs lose water content and become less flexible, they are more prone to tearing or rupturing with even minor strain.
Other causes include:
- Sudden trauma or injury (e.g., car accidents, falls)
- Repetitive motions or heavy lifting
- Poor posture over time
- Obesity, which increases spinal load
- Genetics—some people are more predisposed than others
It’s important to note that many people develop herniated discs without ever experiencing symptoms. Symptoms typically arise when the herniated material presses on nearby nerves.
When Should I See a Doctor?
You should see a physician if:
- Pain lasts more than a few days without improvement
- Pain is severe or worsening
- Numbness, tingling, or weakness occurs
- You have difficulty walking or controlling your bladder or bowels
The last symptom—loss of bladder or bowel control—can indicate cauda equina syndrome, a medical emergency requiring immediate attention.
Even if symptoms seem mild, it’s a good idea to consult a specialist for a proper diagnosis and guidance on treatment options.
How Is a Herniated Disc Diagnosed?
Diagnosis typically begins with a detailed history and physical exam. A doctor may check your reflexes, strength, and sensation to determine if a nerve is being compressed.
Imaging tests may follow:
- MRI (Magnetic Resonance Imaging): Most commonly used; shows soft tissue and nerve detail clearly
- CT scan: Sometimes used if MRI is unavailable
- X-rays: Don’t show discs but may help rule out other spine problems
- EMG (Electromyography): Tests nerve and muscle function if symptoms are unclear
These tools help your provider determine not only if a disc is herniated, but how significantly it’s affecting surrounding structures.
What Are the Nonsurgical Treatment Options?
Most herniated discs improve without surgery. Nonsurgical options may include:
- Activity modification: Avoiding movements that worsen pain
- Physical therapy: Exercises to strengthen supportive muscles and relieve pressure on the spine
- Anti-inflammatory medications: OTC medications like NSAIDs to reduce swelling and discomfort
- Epidural steroid injections: Targeted relief for inflammation around affected nerves
- Hot/cold therapy: Localized temperature changes for temporary symptom relief
These approaches aim to reduce inflammation, improve mobility, and strengthen the body’s ability to support the spine. The majority of patients experience improvement within six to twelve weeks.
When Is Surgery Necessary?
Surgery may be recommended if:
- Nonsurgical treatments fail after several weeks or months
- Pain is severe and limits daily life
- Weakness or numbness is progressing
- There’s loss of bladder or bowel control
The most common surgical procedure is a discectomy, in which the herniated portion of the disc is removed to relieve pressure on the nerve. Minimally invasive techniques now allow for quicker recovery times and less post-operative pain.
Will I Need Physical Therapy After Surgery?
Yes, physical therapy is often part of the recovery process. Post-operative rehab helps:
- Restore strength and flexibility
- Reduce scar tissue formation
- Teach body mechanics to prevent future disc problems
Therapy may begin as early as a few days after surgery, depending on the type and extent of the procedure. Full recovery can take several weeks, but many patients return to normal activities with reduced pain and improved function.
Can a Herniated Disc Return?
It’s possible, though not guaranteed. A previously herniated disc can re-herniate, especially if the underlying risk factors like poor posture, weak core muscles, or heavy lifting aren’t addressed.
Additionally, a herniation in one area increases the likelihood of future disc issues elsewhere along the spine. That’s why long-term maintenance, including exercise and ergonomic adjustments, is key to prevention.
How Can I Prevent Future Disc Problems?
There’s no way to eliminate all risk, but you can significantly reduce your chances of developing another herniated disc by adopting good spinal habits:
- Maintain a healthy weight
- Exercise regularly, focusing on core stability
- Use proper lifting techniques (lift with your legs, not your back)
- Practice good posture, especially when sitting for long periods
- Stay flexible with stretching or yoga
Smoking cessation also helps, as tobacco use can interfere with disc hydration and healing.
Get Answers. Get Relief.
Unexplained back pain, radiating nerve discomfort, or noticeable changes in muscle control could all point to a herniated disc. Left untreated, these symptoms may intensify or lead to long-term damage. However early diagnosis and the right care can make a significant difference.
At Georgia Neurosurgical Institute, we combine advanced diagnostic tools with decades of spine care expertise to uncover the root of the problem and build a treatment strategy that fits your life. From conservative therapies to minimally invasive procedures, our goal is to relieve pressure, restore function, and help you move forward with expert care that’s close to home.
Schedule a consultation with Georgia Neurosurgical Institute today: 478-743-7092
Georgia Neurosurgical Institute offers exceptional treatments for the brain and spine to patients throughout Middle Georgia. With offices in Macon and satellite locations in Dublin, Locust Grove, and Warner Robins, we’re able to treat patients in and around:
- Dublin
- Forsyth
- Locust Grove
- Macon
- McDonough
- Milledgeville
- Perry
- Warner Robins
Recent Articles







