A herniated disc can cause pain, numbness, tingling, or muscle weakness—sometimes in areas far from the spine itself. Recognizing these symptoms early allows for more effective treatment and helps prevent long-term nerve damage. Whether caused by age, injury, or stress on the spine, disc herniation often responds well to conservative care when diagnosed early.
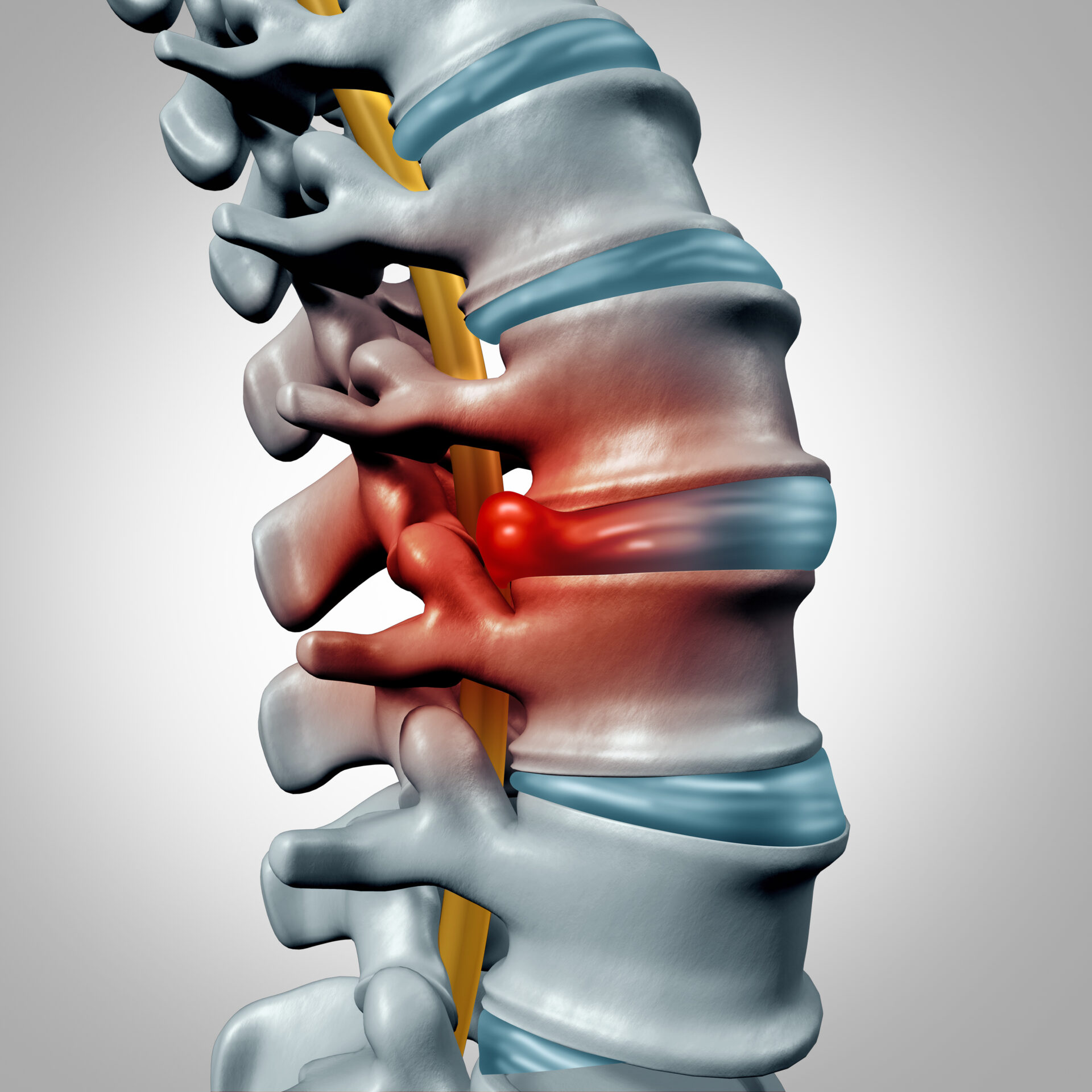
Your spine is made up of a series of bones (vertebrae) separated by flexible, cushion-like discs that act as shock absorbers. These discs allow your spine to bend, twist, and carry the weight of your body. But when one of those discs becomes damaged or moves out of place, it can press against nearby nerves and cause a range of painful and sometimes disabling symptoms.
This condition is known as a herniated disc—and it’s more common than many people realize.
Recognizing the signs of a herniated disc early can make a meaningful difference in both your comfort and your treatment options. Whether you’re dealing with back pain that won’t go away or unusual nerve symptoms in your limbs, here’s how to tell if a herniated disc may be the cause.
What Is a Herniated Disc?
Each spinal disc is made of two parts: a soft inner center (called the nucleus pulposus) and a tougher, fibrous outer layer (the annulus fibrosus). When a disc herniates, part of that soft center pushes through a crack or tear in the outer layer and begins to bulge outward. If the herniation presses against nearby spinal nerves, it can trigger pain, weakness, or numbness that radiates far beyond the spine itself.
Herniated discs most often occur in the lower back (lumbar spine) or the neck (cervical spine), but they can develop anywhere along the spinal column.
While not every herniated disc causes symptoms, many do. Here are the signs that typically bring patients through our doors:
Localized Pain in the Neck or Back
The pain from a herniated disc often begins in the region where the disc has ruptured. If the issue is in the lower back, you may notice a dull ache or sharp pain near the base of the spine, especially after standing or sitting for long periods. If the herniation is in the neck, the pain may radiate across the shoulders or upper back.
This pain may worsen with specific movements—like bending, lifting, coughing, or sneezing—because those actions increase pressure on the spinal column.
Radiating Nerve Pain
When a herniated disc presses on a nerve root, the pain often follows the path of that nerve. This is one of the most distinctive and telling signs of disc herniation.
- In the lower back, pain may travel through the buttock, down the back of the thigh, and into the leg or foot. This is commonly known as sciatica.
- In the neck, the pain may extend from the shoulder into the arm and even into the fingers.
This kind of radiating pain is usually sharp, burning, or electric in nature—and often only affects one side of the body.
Numbness or Tingling
Many patients report a pins-and-needles sensation in the area served by the compressed nerve. This numbness can range from mild to severe, and it may feel like certain parts of your skin are “asleep” or desensitized.
These sensations typically accompany radiating pain but can also occur on their own.
Muscle Weakness or Fatigue
When spinal nerves are compressed for an extended period, the muscles they control can begin to weaken. You might notice:
- Trouble lifting objects you normally carry with ease
- Difficulty gripping things securely
- Loss of coordination or balance when walking
Left untreated, this weakness can worsen and affect your mobility or quality of life.
Loss of Reflexes
A more subtle but clinically important sign of a herniated disc is a reduction in reflexes—such as a slower or absent knee-jerk response. This is something your doctor can test during a physical examination and is often one of the clearest signs of nerve involvement.
Red Flag Symptoms: When to Seek Help Immediately
In rare cases, a herniated disc can cause serious neurological impairment. Call a doctor or go to the emergency room if you experience:
- Sudden loss of bladder or bowel control
- Numbness in the saddle area (inner thighs, back of legs, or around the rectum)
- Severe or rapidly worsening weakness in your legs
These could be signs of cauda equina syndrome, a medical emergency that requires immediate surgical attention.
What Causes a Disc to Herniate?
Herniated discs can develop for many reasons. The most common is age-related wear and tear known as disc degeneration. As we get older, the discs become less flexible and more prone to tearing under even minor strain.
Other contributing factors include:
- Repetitive lifting or twisting motions
- A sudden, awkward movement or fall
- Obesity, which adds pressure to spinal discs
- Smoking, which reduces disc oxygenation and hydration
- Genetic predisposition
Sometimes, a disc can herniate without any clear cause—making it even more important to recognize the symptoms.
How Is a Herniated Disc Diagnosed?
At Georgia Neurosurgical Institute, diagnosis begins with a careful review of your medical history and symptoms, followed by a physical exam. We evaluate your range of motion, reflexes, strength, and areas of numbness or pain.
If symptoms suggest a herniated disc, advanced imaging—such as an MRI or CT scan—can confirm the diagnosis and identify the exact location and severity of the herniation.
Do All Herniated Discs Require Surgery?
No. In fact, most herniated discs can be managed without surgery. Conservative treatment options may include:
- Anti-inflammatory medications
- Physical therapy and guided stretching
- Epidural steroid injections
- Lifestyle modifications (posture, activity, ergonomics)
Surgery becomes an option if:
- Symptoms don’t improve after 6–12 weeks of conservative care
- Pain is severe and limiting your function
- There is significant or worsening neurological weakness
Surgical options—such as microdiscectomy or laminotomy—are often minimally invasive and offer excellent outcomes for the right candidates.
Get Answers. Get Relief.
If you’re experiencing unexplained back pain, nerve symptoms, or changes in muscle strength, a herniated disc could be the cause—and ignoring the signs may allow the problem to worsen. The good news? You don’t have to navigate it alone.
At Georgia Neurosurgical Institute, our experienced spine specialists use advanced imaging and minimally invasive techniques to pinpoint the problem and create a treatment plan tailored to your needs. We’re proud to offer world-class neurosurgical care right here in Middle Georgia—so you don’t have to travel far to get the help you need.
Schedule a consultation with Georgia Neurosurgical Institute today: 478-743-7092
Georgia Neurosurgical Institute offers exceptional treatments for the brain and spine to patients throughout Middle Georgia. With offices in Macon and satellite locations in Dublin, Locust Grove, and Warner Robins, we’re able to treat patients in and around:
- Dublin
- Forsyth
- Locust Grove
- Macon
- McDonough
- Milledgeville
- Perry
- Warner Robins
Recent Articles
- Effective Stretches for Lower Back Pain
- Exercising with Lower Back Pain: What Not to Do
- 5 Ways You Can Make Your Lower Back Pain Worse
- Understanding Different Types of Back Pain







