Discectomy, sometimes spelled diskectomy, is a surgical procedure to alleviate the pain of a herniated disc. Herniation can compress the spinal cord and surrounding nerves, causing significant pain, mobility issues, and other major physical complications. A discectomy allows your surgeon to remove the damaged parts of the disc that are causing nerve pressure to relieve you of pain and other limitations often caused by spinal cord and nerve compression.
While herniation can occur anywhere on the spine, starting at the neck, discs most commonly herniate in the lower back, or the lumbar area.
Disc Herniation, Explained
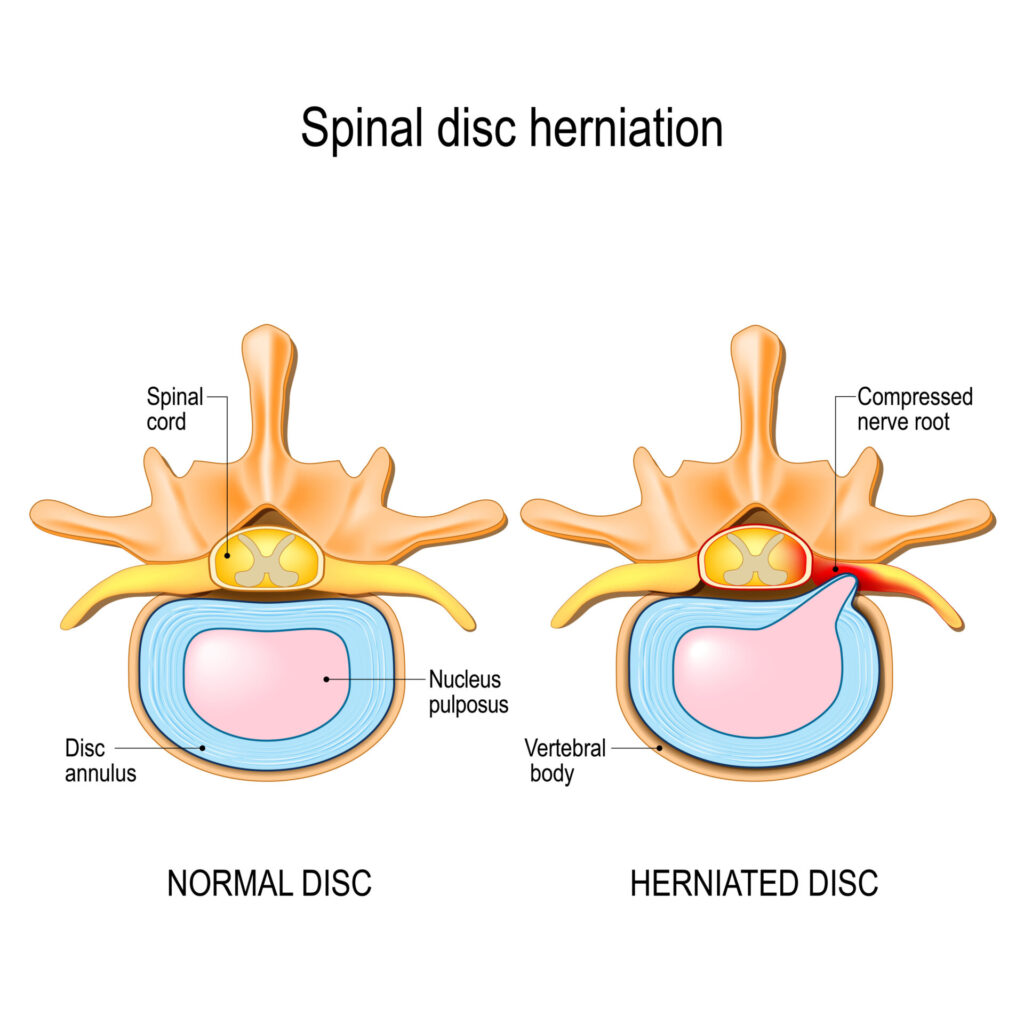
Your spinal discs are cushions between vertebrae, or the backbones that make up your spine, offering crucial shock absorption and spinal flexibility.
Each disc has a rubbery texture and consists of two parts:
- Nucleus pulposus – a jelly-like center designed to enhance the strength, flexibility, and mobility of each vertebra.
- Annulus fibrosis – a barrier around the nucleus made of many layers of collagen fibers. It holds the nucleus pulposus in place, offers stability, and helps minimize compressive stress between vertebrae.
Tears can occur whenever there is damage to the annulus fibrosis, creating room for the nucleus to leak into the spinal canal and compress the spinal cord and connected nerves. This event is called disc herniation (aka slipped or ruptured disc).
Risk Factors that Can Lead to Herniation
Several risk factors can contribute to disc herniation, the most common ones being:
- Age-related wear and tear
- Degenerative disc disease
- Genetics
- Obesity
- Repeated, physically strenuous activity
- Sedentary lifestyle
- Smoking
Symptoms of Disc Herniation
Disc herniation can cause several medical complications in the arms or legs, including:
- Loss of mobility
- Numbness
- Pain
- Tingling
- Weakness
In severe cases of herniation, patients can experience cauda equina syndrome. This severe medical complication affects the cauda equina, or the spinal nerve roots at the base of your spine that resemble a horse’s tail. Damage to this area can lead to incurable nerve issues ranging from permanent weakness to complete leg paralysis.
Signs of cauda equina syndrome include:
- Worsening pain, weakness, or numbness in the pelvis and legs that prevents you from completing regular daily activities and routines
- Loss of bladder or bowel control
- Saddle anesthesia, or loss of feeling in all the areas that touch a saddle—inner thighs, back of the legs, buttocks, and genital region
If you experience symptoms of cauda equina syndrome, seek immediate medical attention. Call 911 or go to an emergency room as soon as possible.
How Does a Discectomy Work?
A discectomy is a procedure that allows your surgeon to clear the spinal canal of any nucleus material that has spilled out from the center of the disc. In ideal cases, only the damaged parts of the disc are removed, but some cases require complete disc removal.
Depending on the location and the severity of the herniation, a laminectomy may precede the discectomy. During a laminectomy, your surgeon removes small amounts of bone and ligament from the surrounding vertebrae to make room in the spinal canal for the discectomy.
Discectomies are considered safe and do not require large incisions to perform, even if a laminectomy is necessary, and are usually recommended after the patient unsuccessfully completes conservative solutions like physical therapy or spinal injections.
Open Discectomy vs. Microdiscectomy
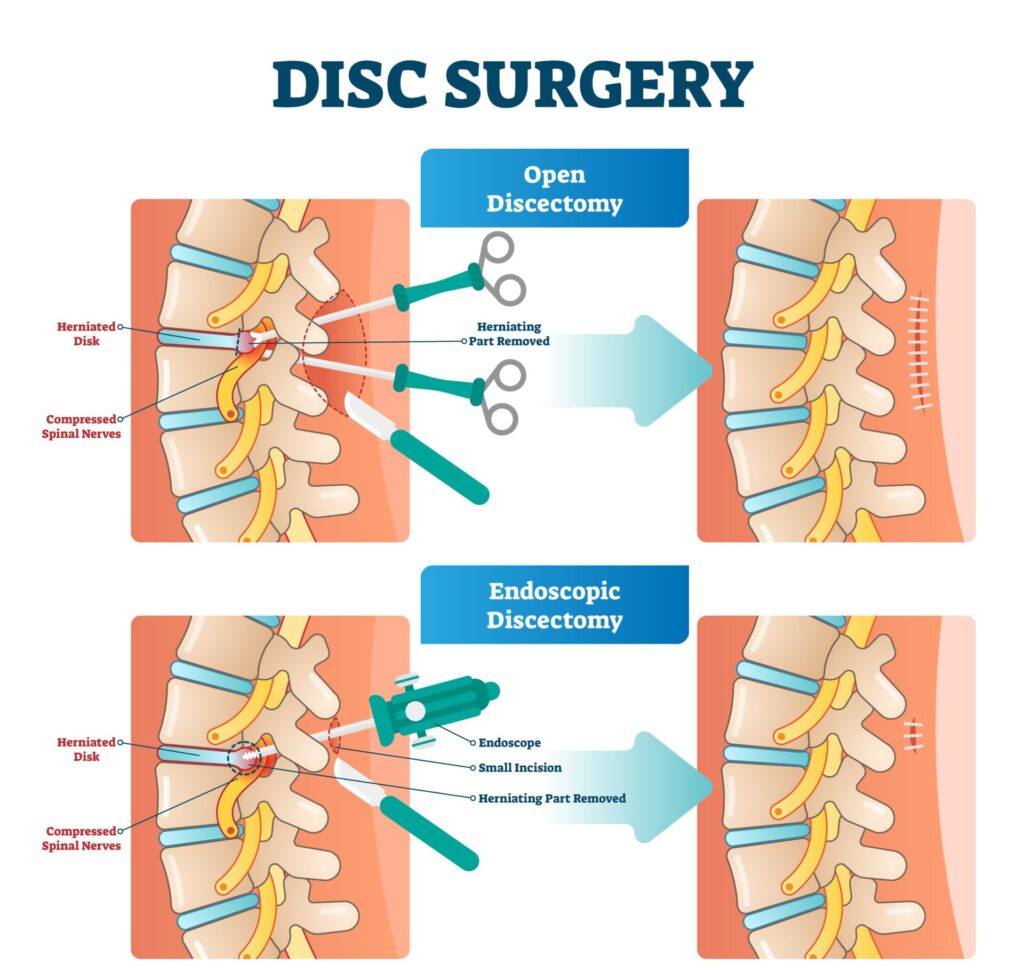
Your surgeon can perform an open discectomy or a microdiscectomy, depending on the severity of your condition:
Open Discectomy: Using general anesthesia, your surgeon will create an incision at the surgery site large enough to access the spine and perform all necessary steps in the procedure, including a laminectomy.
Microdiscectomy: Less invasive than an open discectomy, your surgeon will create a small, 1- to 2-inch incision at the surgery site and perform all steps of the procedure endoscopically.
Discectomy Recovery
Whether you undergo an open discectomy or microdiscectomy, the recovery will look similar:
- Surgery Day to Week 2 – Restrict all activities following surgery.
- Week 2 to Week 6 – Begin taking short walks and drives and perform light activities. Avoid any lifting or strenuous activity. Complete gentle exercises or stretches your doctor recommends. If your occupation allows, you may be able to return to work during this window.
- Week 6 to Week 8 – Begin extending your walking and driving periods. Increase your activity levels, but listen to your body; stop if a movement or exercise is too strenuous. Continue following strength-building regimens assigned by your doctor.
- Week 8 and After – You are usually ready to resume your usual activity by this point.
Patients in Middle Georgia who have experienced disc herniation and want relief may qualify for a discectomy from the expert neurosurgeons at Georgia Neurosurgical Institute.
Our spine specialists are pioneers in surgical technology and bring years of intensive training to deliver successful surgical solutions for your spinal condition. Schedule an appointment with our team today and discover if a discectomy is the right solution for you: 478-743-7092
Thanks for checking out part one of our 3-part series on minimally invasive spinal solutions! Stay tuned for the remaining articles in our series:
- Spinal Solutions: Discectomy
- Spinal Solutions: Laminectomy
- Laminectomy & Discectomy: What Are the Differences?
Related Articles






